Abstract
This study compared the effect of container material type on macronutrient changes in human breast milk (HBM) during frozen storage.
HBM was collected from breastfeeding mothers and baseline macronutrients were analyzed and recorded. The HBM was aliquoted into milk storage containers of five commonly used materials (low-density polyethylene (LDPE), polypropylene (PP), glass, stainless steel, and silicone). The samples were frozen in a standard freezer (-20°F) for 30, 60, and 180 days prior to thawing and retesting macronutrient values.
In the 155 samples analyzed, macronutrient changes among different types of storage materials were insignificant at 30 and 60 days of frozen storage. When comparing macronutrients at baseline to 180 days, there was a significant decrease in protein value over time in LDPE containers as compared to silicone containers (p=0.001). Likewise, there was a significant decrease in total calories from baseline to 180 days in both PP and LDPE containers compared to silicone (p=0.046 and 0.013, respectively).
While not significant for short-term storage, HBM has losses of macronutrients (protein) with long-term storage in LDPE and PP plastics. These differences could have major nutritional impact on growth, particularly to infants born prematurely.
Author Contributions
Academic Editor: Qiuqin Tang, Department of Obstetrics, Nanjing Maternal and Child Health Care Hospital Affiliated to Nanjing Medical University, China.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Marney C. Johnson, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Premature infants, especially extremely low birth-weight infants, receive most of their enteral nutrition in the form of previously frozen, expressed human breast milk (HBM). HBM is the recommended feeding source compared to formula and alternative milk sources 1, 2, 3. It is rich in fat, proteins, and carbohydrates that infants require for growth and prevention of metabolic and endocrine disorders, such as obesity and diabetes.4,5,6,7,8 It also provides critical maternal antibodies and other immune system elements, such as lactoferrin and secretory Immunoglobulin A (IgA).9 Breastfeeding exposes the infant to beneficial bacteria and enzymes important to the developing digestive system, as well as stimulates a tolerance to potential food allergens. 1, 2, 3,10, 11
When calculating the amount of HBM to feed Neonatal Intensive Care Unit (NICU) patients, neonatologists use an assumed value of 20 calories per ounce. However, recent clinical trials demonstrated discrepancies in the assumed value of 20 calories per bounce. Even though both NICUs used identical models of near infrared milk analyzers calibrated with the same donor milk samples, samples from participants in one center were consistently lower in caloric content than their counterparts.12
While research has shown changes in macronutrient levels in HBM as a result of freezing, thawing, and warming the milk,7,13 very little has been done to investigate the role of the storage container in the loss of macronutrients. This leads to the question: Is our current practice of storing HBM in polypropylene plastic bottles causing alterations in the milk and its macronutrients?
While another study showed that 48-hour frozen storage of previously refrigerated term HBM decreases its percentage of fat, it also noted an increase in carbohydrates and protein, leading to only a slight decrease in calories that did not reach statistical significance.14 It is recommended that NICU facilities store frozen expressed HBM at -20°C and therefore, storage temperature can effectively be eliminated as a confounding factor 15. The most variable factor between milk storage in the NICU and in the home is the type of containers used. Therefore, further investigation was needed to examine what type of container best preserves HBM macronutrients.
Preterm infants are often fed expressed HBM, often previously frozen and derived from their own mothers or donated term milk, and therefore it is of the utmost importance to maximize nutrient preservation. Preterm HBM has more protein and fat and typically fewer carbohydrates compared to term HBM;16 however, due to increased nutrient demands, minimal alterations can have a profound impact in very small infants who depend on this type of nutrition and milk storage for months. In this study, we hypothesized macronutrient differences exist depending on the type of HBM storage container utilized. Secondly, we hypothesized that the container material has a greater effect on macronutrient loss with prolonged storage. This study is innovative in that it analyzed samples frozen for extended time periods more typical for normal use of frozen HBM. Additionally, this study includes analysis of stainless steel and silicone, which, to our knowledge, have never been assessed for frozen storage of HBM.14,15,1, 6,1, 7
Materials and Methods
Participants
Mothers who delivered at University Health System in San Antonio in 2016 were enrolled in this study. Age, race, ethnicity, and socioeconomic data were not collected, and the presence of mastitis and other local or systemic infections that alter the content of milk was the only exclusion criteria. Patients were enrolled at 2 to 30 days postpartum, and were producing sufficient HBM so that the study would not impact their infants’ ability to receive their mothers’ milk. Lactation specialists instructed participants in proper breast milk expression techniques, including expression of hind milk to obtain maximal nutritional content. Participants were permitted to donate up to three separate milk samples within a 10-day period. Of the 8 participants enrolled, one was unable to donate a sample due to inadequate milk production.
Sample Collection
Participants expressed breast milk via mechanical or hand expression into glass bottles on-site at the NICU or Newborn nursery. Up to three 25-30 milliliters (ml) samples were collected from each participant. Samples were collected by the research team within 15 minutes and processing began immediately.
Sample Processing
Each sample was assigned a de-identified study number and gently hand-agitated prior to processing. For consistency, all collection bottles, pipettes, and test tubes were glass. A baseline sample was obtained and processed: 3 ml was homogenized with a probe sonicator (QSonica, Newtown, CT) for 7 seconds. One ml of homogenized milk was analyzed for macronutrient content (fat, protein, carbohydrate, and calculated caloric content) using a near infrared milk analyzer (Spectrastar 2400RTW; Unity Scientific, Brookfield, CT).
Remaining un-homogenized milk was aliquoted in 3 ml portions to containers made of materials commonly used for HBM storage; (a) Low-density polyethylene or LDPE (Pump & Save breast milk bags, Medela, McHenry, IL), (b) Polypropylene (VoluFeed, Abbott, Lake Forest, IL), (c) Food-grade stainless steel (Kiki, Pura Stainless, Santa Barbara, CA), (d) Food-grade silicone [BabyPods, Mastrad Inc., Paris, FR), and (e) borosilicate glass (Avent Natural baby bottle, Philips, Sudbury, UK).
Care was taken to pipette samples directly to the bottom of the storage vessel and to prevent contact between the sample and container lid throughout the study. Samples were frozen in whole form (unsonicated, raw, whole milk) and stored in a domestic freezer (Kenmore Elite 17802, Sears, Roebuck and Co., Chicago, IL) at -20°F for 30, 60 (average time of use), and 180 days (“optimal” maximum recommended frozen storage time).18
Samples were removed from frozen storage on or within one day of intended retesting date, thawed to room temperature for 45 minutes in room air, gently agitated, transferred with glass pipettes into glass test tubes, homogenized, and analyzed as previously described for baseline samples. Residual sample was stored in non-reactive glass at -80°C.
Statistical Analysis
Statistical calculations were performed with SPSS for Windows v 24.0 (SPSS, Inc., Chicago, IL). Macronutrients for each type of container were determined to be normally distributed from the fat, protein, carbohydrate, and calory content measured on each of the samples using a Shapiro-Wilk test. Differences between and within groups were analyzed using One-way ANOVA followed by Bonferroni’s or Tukey’s test and regression analysis, as appropriate. A value of p < 0.05 was considered statistically significant. Levine’s test was performed to assess subject variability.
Results
In total, 9 mothers were approached for recruitment; of these, one declined to participate. Of the 8 mothers recruited, one was unable to donate due to insufficient milk production. Therefore, 7 mothers (2 term and 5 preterm) donated 8 bottles of milk. These samples were divided and resulted in 155 individual samples to be analyzed at baseline, 30, 60, and 180 days of frozen storage with each container tested; the minimum number of samples for each time-point was 5. One of the mothers provided a slightly decreased volume of milk and, therefore, we were unable to complete the expected samples to be aliquoted.
The macronutrient analyses from each type of container at each time point are shown in Table 1. There was no difference in the amount of fat or total calories between the different containers utilized at 30, 60, or 180 days of storage. Protein content remained similar between all types of containers at 30 and 60 days, whereas it was lower in LDPE vs silicone at 180 days (p=0.036). The amount of carbohydrates at 30 and 60 days remained similar but was elevated in the silicone container compared to stainless steel at 180 days (p=0.04).
Table 1. Macronutrient values of breast milk over time at -20°F| Silicone | Glass | Stainless Steel | Polypropylene | LDPE | ||
| Fat (g/dL) | ||||||
| Baseline | 3.5 ± 1.5 | 3.5 ± 1.5 | 3.5 ± 1.5 | 3.5 ± 1.5 | 3.5 ± 1.5 | |
| 30 days | 3.2 ± 1.4 | 3.2 ± 1.4 | 3.3 ± 1.4 | 3.1 ± 1.3 | 3.3 ± 1.5 | |
| 60 days | 3.0 ± 1.4 | 3.0 ± 1.3 | 3.2 ± 1.4 | 3.2 ± 1.4 | 2.9 ± 1.2 | |
| 180 days | 3.5 ± 1.5 | 3.4 ± 1.4 | 3.5 ± 1.6 | 3.3 ± 1.4 | 3.5 ± 1.4 | |
| Protein (g/dL) | ||||||
| Baseline | 1.0 ± 0.2 | 1.0 ± 0.2 | 1.0 ± 0.2 | 1.0 ± 0.2 | 1.0 ± 0.2 | |
| 30 days | 1.0 ± 0.1 | 1.0 ± 0.1 | 0.9 ± 0.1 | 0.9 ± 0.2 | 1.0 ± 0.2 | |
| 60 days | 0.9 ± 0.2 | 0.9 ± 0.2 | 1.0 ± 0.2 | 0.9 ± 0.2 | 1.0 ± 0.2 | |
| 180 days | 1.1 ± 0.2 | 1.0 ± 0.2 | 1.0 ± 0.1 | 0.9 ± 0.2 | 0.8 ± 0.2* | |
| Carbohydrates (g/dL) | ||||||
| Baseline | 7.3 ± 0.3 | 7.3 ± 0.3 | 7.3 ± 0.3 | 7.3 ± 0.3 | 7.3 ± 0.3 | |
| 30 days | 7.3 ± 0.5 | 7.2 ± 0.2 | 7.3 ± 0.2 | 7.3 ± 0.4 | 7.4 ± 0.4 | |
| 60 days | 7.5 ± 0.3 | 7.3 ± 0.3 | 7.3 ± 0.3 | 7.2 ± 0.2 | 7.3 ± 0.2 | |
| 180 days | 7.5 ± 0.3 | 7.5 ± 0.2 | 7.2 ± 0.2‡ | 7.3 ± 0.2 | 7.4 ± 0.2 | |
| Calories (kcal/oz) | ||||||
| Baseline | 19.0 ± 4.1 | 19.0 ± 4.1 | 19.0 ± 4.1 | 19.0 ± 4.1 | 19.0 ± 4.1 | |
| 30 days | 18.3 ± 3.7 | 18.0 ± 3.8 | 18.5 ± 3.8 | 17.9 ± 3.6 | 18.5 ± 4.4 | |
| 60 days | 17.9 ± 3.7 | 17.6 ± 3.4 | 18.2 ± 3.8 | 18.1 ± 3.6 | 17.3 ± 0.2 | |
| 180 days | 19.4 ± 3.7 | 18.9 ± 3.7 | 18.9 ± 4.1 | 18.5 ± 3.7† | 19.0 ± 3.6† | |
The relationship between storage time for each type of container by regression analysis can be seen in Figure 1; there is a tendency for fat and total calories to remain relatively stable during storage, while protein tends to decrease, and carbohydrates tend to increase, but this did not reach statistical significance from baseline.
Figure 1.Linear regression of frozen milk macronutrient analysis Linear regression of the macronutrient trends over time in frozen storage per material type. Dots represent means per time point and shaded regions show the confidence levels.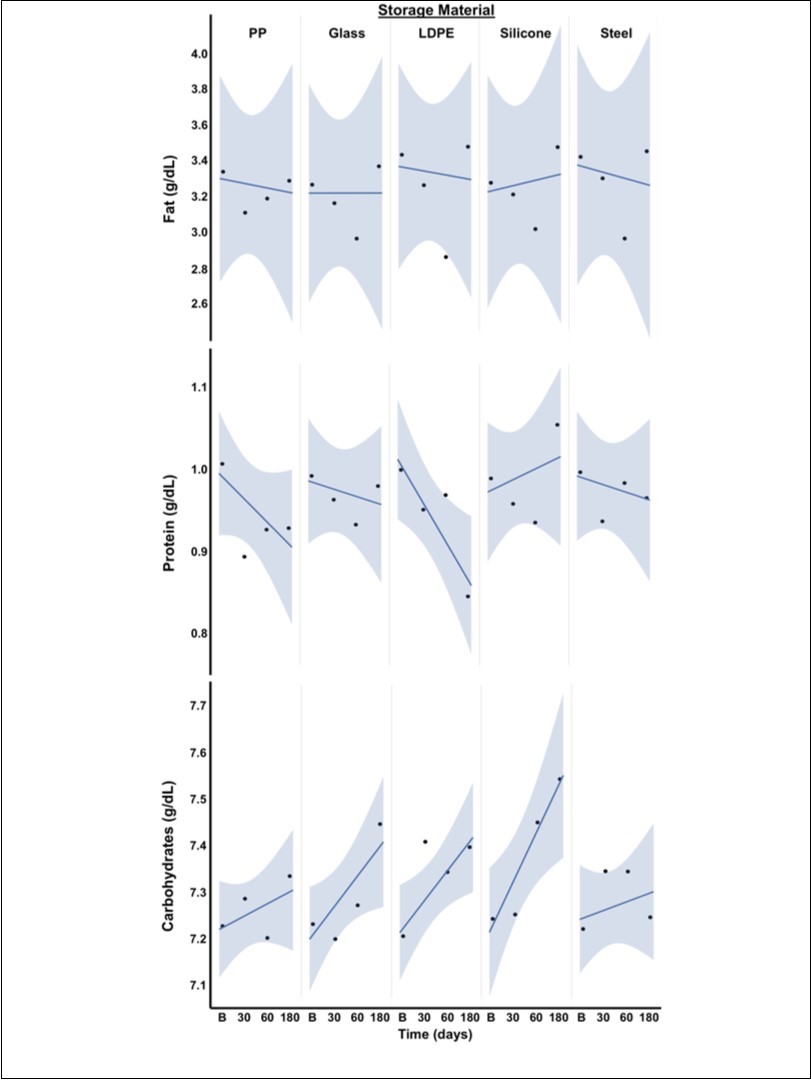
When examining change from baseline, fresh milk to 180 days of frozen storage, silicone retained significantly more protein than the LDPE container (p=0.001) and more total calories (kcal/oz) than polypropylene and LDPE containers (p=0.046 and 0.013, respectively) (Table 1).
Discussion
In this study, we demonstrated that LDPE might have a detrimental effect on HBM macronutrient content with long-term storage. LDPE bags are widely used due to their low cost, portability, accessibility, and economic utilization of freezer storage space. LDPE bags have been rapidly adopted for easy use at home and it is uncertain how often they are used both inpatient and outpatient. The findings of this study demonstrate that the cost to the infants’ nutrition may be high: such a great loss of protein will inevitably have a negative impact on the growth of the baby. Head circumference, linear growth, and short-term weight gain is greatly impacted by enteral protein intake.19,20 Several studies have shown that for the extremely low birth weight (ELBW) infant, increased weight gain has a positive effect on neurodevelopment21,22and decreases rehospitalization rates,23 making protein a vital component of the premature infant’s ongoing health. A premature infant would receive on average, 0.2 grams (g) per deciliter (dL) less protein if LDPE containers were utilized for milk storage. That is, an infant with a minimum intake of 150ml/kg/day would receive approximately 0.3g/kg less protein per day (10% less than the recommended protein intake); a cumulative loss of 9g/kg of protein in a 30 day period. Therefore, a higher daily intake of HBM may be required to account for protein losses and to meet full nutritional needs.
Contrary to what we expected, LDPE containers showed stable fat content. Previous studies have shown a loss of fat to plastic used for continuous tube feeding, which their authors speculated was due to the plastic containers causing fat globules to adhere to their surfaces.24,25 We speculate that our samples did not experience similar fat loss due to the small sample volumes and the careful thawing and sampling procedures implemented in a controlled research environment. This would indicate that the loss of fat in continuous feed setups is likely due to the length of time the milk is sitting in the apparatus, or the structure of the apparatus itself. Further research is needed to examine the connection between fat loss and gravity-based continuous feeds versus bolus feeds, length of feed tubing, etc.
Additionally, LDPE bags showed an upward trend in carbohydrate content over time. The net effect of this loss of protein and apparent gain in carbohydrates translated into stable caloric content over time, but this maintenance of calories should not be confused with maintaining the quality and integrity of milk and its components. It is unclear at this time why there is such a significant loss of protein in LDPE bags, meriting further research. One may speculate that their zip-top seals do not create an adequate seal or that the thinness of the material allows the milk to freeze too quickly; perhaps one or both of these encourage proteolysis, increases precipitation, or cause protein to adhere to the surface of the container.
The second container we tested was silicone. We chose silicone as it is rising in popularity for home breast milk storage because its ability to be reused appeals to the environmentally conscious and it is generally considered a safe alternative to plastics. Samples stored in silicone containers showed a significant increase in carbohydrate content at 180 days as compared to stainless steel. The reason for this increase in carbohydrates is not clearly established; it may be an inherent unreliability of near-infrared milk analyzers, the result of the high quantities of oligosaccharides present in human breast milk, which “contain a terminal lactose molecule and its spectral absorption cannot be differentiated from that of free metabolizable lactose.26” However, another possibility exists: this discrepancy may be the result of variability in the strength of an airtight seal. While silicone can create an airtight seal for a hard container, we found it was much more difficult to maintain a seal on a silicone-walled vessel, as a relatively light touch could cause the soft sides to push the lid out. While care was taken to transport and store the silicone vessels in such a way to prevent this, perhaps this weaker seal plays a role in the overall increase in carbohydrates. The samples stored in silicone were otherwise relatively stable in protein and fat, resulting in only a minor upward trend in caloric content. Because of this, further research is needed to help us understand if it is indeed a reliable alternative, or if this upward trend in carbohydrates indicates an undesirable change.
We also chose to study polypropylene because it is the material of which our NICU's bottles are made. Polypropylene (PP) is a cost-effective material and its solid structure and light weight make a convenient and inexpensive bottle with which to provide our patients. PP demonstrated a downward trend in protein content over time, but was not significant. While a significant difference was observed between silicone and PP in caloric content from baseline to 180 days, we suspect that this relationship is due in large part to the carbohydrate increase over time in silicone containers, as previously discussed.
Much like silicone, glass containers were chosen for this study due to their increasing popularity for home use as an inert and reusable storage container. In glass containers, carbohydrate content trended upward over time, but did not reach significance. As previously discussed, future research into the reasons and value of the changes to protein and carbohydrates will help to determine whether polypropylene or glass vessels are better for long-term storage.14,17,26
Stainless steel was also chosen due to its growing popularity for at-home use; not only for its reusable and chemically-inert properties, but because it is lighter weight and stronger than glass. Stainless steel appears to maintain the most stable macronutrient content in HBM. When compared to other containers, it had a significantly lower amount of carbohydrates than silicone at 180 days, but the total amount of carbohydrates had increased over time in the silicone bottle, likely due to evaporation or inaccuracy of measurements. From baseline to 180 days of frozen storage, stainless steel had no significant changes in fat, protein, or carbohydrate content, nor did it demonstrate any strong trends that would seem to demand a larger sample size to confirm. Its apparent protective effects could make stainless steel a beneficial storage container for NICU or home use. However, stainless steel containers are more expensive, and the inconvenience and labor cost of cleaning and sterilizing reusable bottles makes them more difficult to utilize in a hospital setting.
One of the limitations to this study included donor number and the method of analyzing macronutrients. Near infrared milk analyzers may not be the most accurate way to analyze macronutrients in milk, though it is fast and convenient for hospital use.26 Another limitation was that we were not able to collect demographic characteristics of the participants due to the Institutional Review Board approval of this study as exempt.
Most of the findings suggest the type of container matters with long term storage. As this is a common practice with premature infants, labeling the time of milk collection of human milk is of utmost importance, in particular when utilizing LDPE bags. Prompt use (<60 days) should be encouraged if LDPE bags are utilized for storage.
Conclusion
This study found differences between the type of container used and macronutrient integrity of human milk. In particular, we found LDPE bags to have less protein and total calories than other frequently used types of containers with prolonged storage. Therefore, storage of human milk in LDPE bags for more than 60 days should be discouraged, in particular in the setting of prematurity as it can translate into poor growth and decreased protein intake in premature infants.
Acknowledgments
We would like to thank the University Hospital NICU dietitians for their contribution in screening mothers for study recruitment. We would also like to express our sincere appreciation to the participants for their donation of expressed breast milk for this research project.
References
- 1.Reeves A A, Johnson M C, Vasquez M M. (2013) TGF-beta2, a protective intestinal cytokine, is abundant in maternal human milk and human-derived fortifiers but not in donor human. 8(6), 496-502.
- 2.Sullivan S, Schanler R J, Kim J H. (2010) An exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products.JPediatr156(4):. 562-567.
- 3.Cristofalo E A, Schanler R J, Blanco C L. (2013) Randomized trial of exclusive human milk versus preterm formula diets in extremely premature infants,J Pediatr163(6):. 1592-1595.
- 4.Ehrenkranz R A.Early nutritional support and outcomes. in ELBW infants.Early Hum Dev2010;86 Suppl 1, 21-25.
- 5.Dusick A M, Poindexter B B, Ehrenkranz R A. (2003) Growth failure in the preterm infant: Can we catch up?Semin Perinatol27(4):. 302-310.
- 6.Ehrenkranz R A, Dusick A M, Vohr B R. (2006) Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants.J. 117(4), 1253-1261.
- 7.Savino F, Liguori S A, Fissore M F. (2009) . Breast Milk Hormones and Their Protective Effect on Obesity. IntJPediatrEndocrinol2009: 327505.
- 8.Victora C G, Bahl R, Franca G V. (2016) Breastfeeding in the 21stcentury: epidemiology, mechanisms, and lifelong. 387(10017), 475-90.
- 9.Handa D, Ahrabi A F, Codipilly C N. (2014) Do thawing and warming affect the integrity of human milk?J. 34(11), 863-866.
- 10.Namachivayam K, Blanco C L, Frost B L. (2013) Preterm human milk contains a large pool of latent TGF-beta, which can be activated by exogenous neuraminidase.Am. 304(12), 1055-65.
- 11.Munblit D, Peroni D G, Boix-Amorós A. (2017) Human Milk and Allergic Diseases: An Unsolved Puzzle.Nutrients9(8):. 894.
- 12.Hair A, Blanco C, Moreira A. (2014) Randomized Trial of Human Milk Cream as a Supplement to Standard Fortification of an Exclusive Human Milk-Based Diet in Infants 750-1250 g. , Birth Weight.J 165(5), 915-920.
- 13.Thatrimontrichai A, Janjindamai W, Puwanant M. (2012) Fat loss in thawed breast milk: Comparison between refrigerator and warm water.Indian Pediatr49(11):. 877-880.
- 14.Chang Y, Chen C, Lin M. (2012) The macronutrients in human milk change after storage in various containers.PediatrNeonatol53(3):. 205-209.
- 15.Bankhead R, Boullata J, Brantley S, Corkins M, Guenter P. (2009) Enteral nutrition practice recommendations. , JPEN Parenter Enteral Nutr 33(2), 122-167.
- 16.Gidrewicz D A, Fenton T R. (2014) A systematic review and meta-analysis of the nutrient content of preterm and term breast milk.BMC. Pediatr14: 216.
- 17.Janjindamai W, Thatrimontrichai A, Maneenil G. (2013) Soft plastic bag instead of hard plastic container for long-term storage of breast milk.Indian. 80(10), 809-813.
- 18. (2017) The Academy of Breastfeeding Medicine Protocol Committee. ABM Clinical Protocol #8: Human Milk Storage Information for Home Use for Full-Term Infants. Available: http://www.bfmed.org/Resources/Protocols.aspx.
- 19.Dogra S, Thakur A, Garg P. (2017) . Effect of Differential Enteral Protein on Growth and Neurodevelopment in Infants <1500 g: A Randomized Controlled Trial.JPediatrGastroenterolNutr 64(5), 126-132.
- 20.Kuschel C, Harding J. (2000) Protein supplementation of human milk for promoting growth in preterm infants.Cochrane Database Syst Rev(2):CD000433.
- 21.Strommen K, Blakstad E W, Moltu S J. (2015) Enhanced nutrient supply to very low birth weight infants is associated with improved white matter maturation and head growth. , Neonatology 107(1), 68-75.
- 22.Belfort M B, Rifas-Shiman S L, Sullivan T. (2011) Infant growth before and after term: effects on neurodevelopment in preterm infants. , Pediatrics 128(4), 899-906.
- 23.Ehrenkranz R A, Duscik A M, Vohr B R. (2006) Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants.Pediatrics117(4):. 1253-61.
- 24.Mokha J S, Davidovics Z H. (2017) Improved Delivery of Fat From Human Breast Milk via Continuous Tube Feeding. , J Parenter Enteral Nutr 41(6), 1000-1006.
